We often get questions about why we monitor bloodwork during chemotherapy treatment. Here is some information about why we do this, and what the different blood tests mean.
Why does my pet need blood testing before and after chemotherapy?
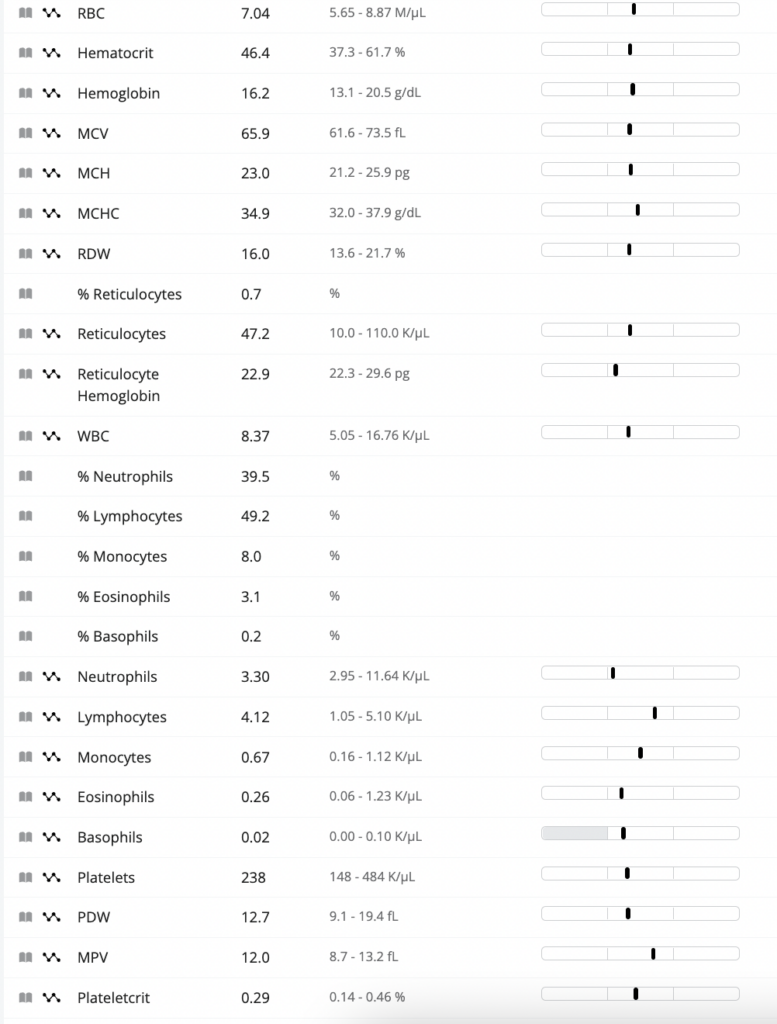
Most chemotherapy medications can cause bone marrow suppression as a potential side effect. Our bone marrow makes red blood cells, white blood cells, and platelets. All of these blood cells have different and very important functions. We measure the blood cell levels with a test called a complete blood count, or a CBC. A CBC looks like this:
What do the parameters and numbers on the CBC mean?
There are many numbers to look at on a CBC! Here we will guide you through the different blood cell types, along with some of the more important parameters we look at for chemotherapy patients:
Red Blood Cells:
Red blood cells (also known as erythrocytes) carry oxygen from the lungs to other tissues in the body, and return carbon dioxide from other tissues in the body to the lungs. On the CBC, we mainly look at the hematocrit to monitor the red blood cell level. We may also run an in-house test called a packed cell volume (PCV) to more precisely assess a patient’s red blood cell level.
Although there are some conditions that can cause an erythrocytosis (increased red blood cell level), in most chemotherapy patients we monitor for anemia (decreased red blood cell level). If a patient is anemic, there are additional parameters on the CBC (MCV, MCHC, hemoglobin, reticulocytes) that we look at to help determine the cause of the anemia, and how effectively the bone marrow is working to correct it.
In general, anemia can occur due to three broad causes- decreased production of red blood cells, destruction of red blood cells, or loss of blood. There are many possible specific causes of anemia in dogs and cats, and understanding the cause of the anemia is important in determining the best way(s) to treat it. In cases where the anemia is mild or moderate, we may monitor the trend of the anemia over several blood tests before changing treatment. Many patients who are taking chemotherapy develop a mild anemia over time, which is generally not harmful.
If you notice that your dog or cat has pale or white gums, is unsteady or weak on their feet, or breathing rapidly, please seek veterinary care right away. These signs can indicate a severe anemia, which can be life-threatening if left untreated.
White Blood Cells:
White blood cells (also known as leukocytes) make up an important part of the immune system. There are many different types of white blood cells with varying functions, and the ones we measure on the CBC are neutrophils, lymphocytes, monocytes, eosinophils, and basophils.
Neutrophils are one of our earliest responders to infections. They are short-lived immune cells (hours to a day), and are continuously produced by the bone marrow. Since many chemotherapy medications preferentially target rapidly dividing cells, sometimes a chemotherapy treatment will transiently drop the neutrophil count.
When your pet comes in for a chemotherapy treatment in the hospital, we will check to make sure he or she has enough neutrophils for treatment. If the neutrophil count is too low, we will delay treatment in order to give the bone marrow more time to recover. A low neutrophil count (also called neutropenia) usually self-corrects within a few days or a week. If the neutrophil count is very low (usually <1k/uL), we will have your pet take a short antibiotic course in order to help guard against opportunistic infections until the neutrophil count returns to normal.
Rarely, patients with a low neutrophil count can develop a fever and a systemic infection. This is called febrile neutropenia. If this happens, it can be very serious if left untreated- however, most patients with febrile neutropenia recover quickly with intravenous fluids, antibiotics, and good supportive care.
An increased neutrophil count (also called neutrophilia) can be seen with infection, inflammation, or certain other conditions.
Lymphocytes are a large family of white blood cells that have lots of different functions! This group of white blood cells includes B cells, helper T cells, killer T cells, and regulatory T cells, among others. In oncology patients, we typically are not concerned if the lymphocyte count is low. If we notice an increased lymphocyte count (lymphocytosis), it is wise to investigate further. An elevated lymphocyte count can be seen with certain infections, certain types of cancer, and rarely other conditions.
Monocytes are a group of white blood cells that participate in something called antigen presentation, which is a way that certain immune system cells communicate with each other about potential threats in the body. In oncology patients, it is more concerning if the monocyte count is very high (monocytosis) than if it is decreased. While a mild monocytosis is not an automatic cause for concern, a significant monocytosis warrants further investigation.
Eosinophils are a type of immune cell that is important in immune response to parasitic infestations, as well as allergies. A low eosinophil count is generally not worrisome, whereas a high eosinophil count can be seen with parasitic infestations and certain types of cancer (such as a mast cell tumor).
Basophils are one of the more mysterious white blood cell types- we don’t know as much about them as we do about some of the others. We do know that they are important in our response to parasitic infestations, and that they have a role in allergic responses as well. A low basophil count is typically not of concern, whereas it is recommended to investigate a significantly increased basophil count.
Although a full discussion of all of the different immune cell subtypes and their functions is beyond the scope of this resource, more detailed information can be found here (or ask Dr. MaloneyHuss when you are in for your appointment, she loves immunology nerd time!).
Platelets:
Platelets are cells that help us to clot our blood. They have a lifespan of about 7 days, and (similar to neutrophils) we can see transient decreases in the platelet count after chemotherapy administration. If the platelet count is low on the CBC, we typically will perform a manual platelet count. This involves preparing a blood smear and visually counting the platelets under the microscope, as well as checking for platelet clumps. Since platelets are naturally sticky, they sometimes clump up as the blood is being analyzed and cause the platelet count to be spuriously decreased. Performing a blood smear allows us to verify if the platelet count is truly decreased, or if the decrease is due to clumping.
Patients with a decreased platelet count (thrombocytopenia) secondary to chemotherapy administration will typically self-correct back to a normal platelet count in a week or two. If the thrombocytopenia persists beyond that, we may recommend checking for other causes of a low platelet count (such as certain tick-borne diseases, cancers, or autoimmune conditions).
Patients with a markedly decreased platelet count (<50,000/uL) are at particular risk for bleeding. If you notice pinpoint bruises or blood spots on the gums or skin, bleeding from the nose or mouth, coughing blood, or blood in the front of the eyes, please seek veterinary care at once.
It is typically not concerning for patients to have a platelet count that is increased above the reference range (thrombocytosis)- from what we know, these patients are not at an increased risk of clot formation due to the elevated platelet count! If a patient has a severe, persistent thrombocytosis (>1,000,000/uL), further evaluation is recommended.
My pet also had a test called a chemistry screen. What is this?
A chemistry screen (also called a blood chemistry or a metabolic panel) evaluates parameters of organ function, blood proteins, and electrolytes. A chemistry screen looks like this:
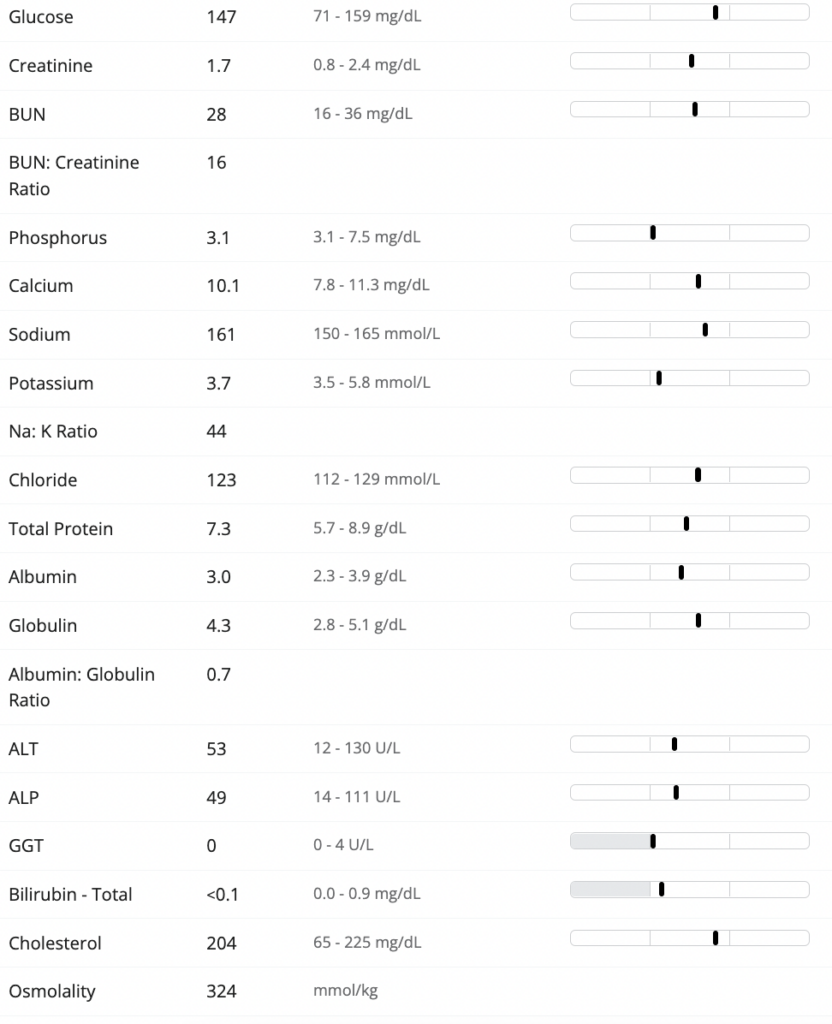
As you can see, there are many parameters on a chemistry screen- and most of them are best interpreted in relevant subsets rather than individually.
We typically will look at BUN, creatinine, and another parameter called SDMA (not listed on the above chemistry screen) to evaluate kidney function, in addition to phosphorus, potassium, calcium, and albumin. For liver health, we often look at ALT, ALP, GGT, and bilirubin, as well as glucose, cholesterol, BUN, and albumin.
Certain diseases, cancers, and cancer treatments can affect the electrolytes in the blood, and a chemistry screen is an important way to monitor these parameters over time.
Although full interpretation of a chemistry screen is beyond the scope of this resource, more detailed information can be found here on the individual parameters and their interpretation.
Why does my pet need so many blood tests? Can my primary care vet do any of these?
Each chemotherapy protocol has its own blood testing schedule, based on which organs the chemotherapy may affect, and how suppressive the chemotherapy is to the bone marrow. Your pet’s bloodwork schedule will then be adjusted based on any other health problems they have, in order to make sure all of them are being monitored appropriately.
Oftentimes, interim bloodwork between chemotherapy doses can be performed by a patient’s primary care veterinarian and sent to your oncologist for review. If it’s closer, less expensive, and/or easier for you to visit your primary care veterinarian, please let us know. We will plan to check ahead of time to be sure your primary care veterinarian is comfortable with the specific diagnostics and plan that are recommended for your pet.